The human body constantly exchanges gases and eliminates waste products to maintain life. The respiratory system ensures oxygen supply and carbon dioxide removal, while the urinary system filters blood and maintains fluid, electrolyte, and acid–base balance.
Respiratory System
The respiratory system is a biological system that facilitates gas exchange. It’s responsible for taking in oxygen from the environment and releasing carbon dioxide from the body.
Mechanism of Respiration
Respiration, or breathing, is a two-part mechanical process: inhalation and exhalation.
- Inhalation: This is an active process. The diaphragm contracts and moves downward while the intercostal muscles contract, lifting the ribs and sternum upward and outward. This increases the volume of the chest cavity, causing a drop in internal pressure. Air then rushes into the lungs to equalize the pressure.
- Exhalation: This is typically a passive process. The diaphragm and intercostal muscles relax, decreasing the volume of the chest cavity. The increased pressure inside the lungs forces air out. During forced exhalation (e.g., exercise), the abdominal muscles also contract to push more air out.
Regulation of Respiration
Breathing is primarily controlled by the respiratory center located in the medulla oblongata and pons of the brainstem. This center sends signals to the diaphragm and intercostal muscles to control the rate and depth of breathing. Chemoreceptors in the brain and blood vessels monitor the levels of carbon dioxide (CO2), oxygen (O2), and pH.
- The most important factor in regulating breathing is the concentration of CO2. An increase in blood CO2 levels leads to a drop in pH, which is detected by chemoreceptors. This signals the respiratory center to increase the breathing rate to expel more CO2.
- A decrease in blood O2 levels is a less potent stimulus for breathing but is important in conditions like chronic lung disease.
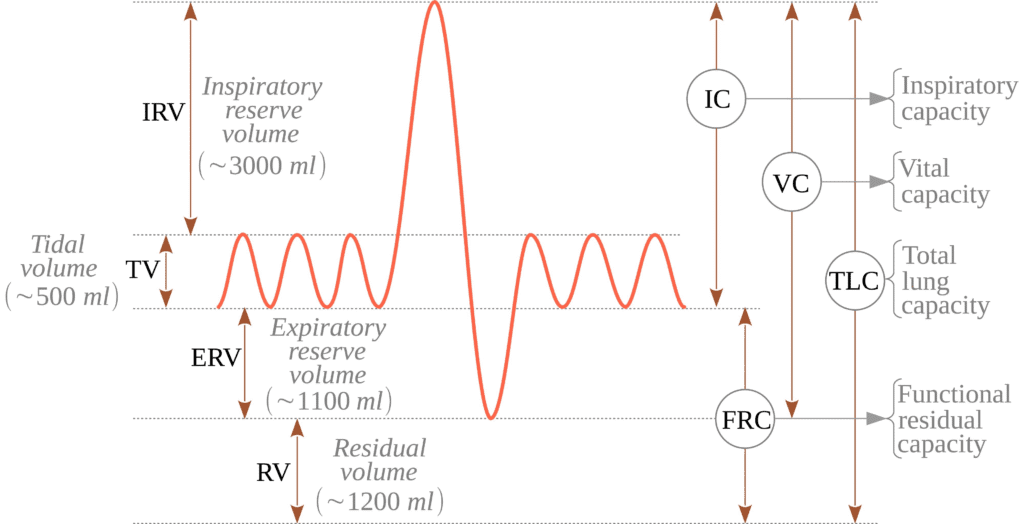
Lung Volumes & Capacities
Lung volumes measure the amount of air in the lungs at different stages of the respiratory cycle. Lung capacities are the sums of two or more volumes.
- Tidal Volume (TV): The amount of air inhaled or exhaled during a normal, quiet breath (approx. 500 ml).
- Inspiratory Reserve Volume (IRV): The maximum amount of air that can be inhaled after a normal inspiration.
- Expiratory Reserve Volume (ERV): The maximum amount of air that can be exhaled after a normal expiration.
- Residual Volume (RV): The amount of air that remains in the lungs even after a maximal exhalation.
- Vital Capacity (VC): The total amount of air that can be exhaled after a maximal inspiration. VC=TV+IRV+ERV.
Transport of Respiratory Gases
Oxygen and carbon dioxide are transported through the blood.
- Oxygen Transport: About 97% of oxygen is transported by hemoglobin in red blood cells, which forms oxyhemoglobin. The remaining 3% is dissolved in the blood plasma.
- Carbon Dioxide Transport:CO2 is transported in three main ways:
- As bicarbonate ions (HCO3−) (approx. 70%), which is the primary method.
- Bound to hemoglobin (as carbaminohemoglobin) (approx. 23%).
- Dissolved in the blood plasma (approx. 7%).
Urinary System
The urinary system is a group of organs that produce, store, and eliminate urine. Its main function is to filter waste products from the blood and regulate the body’s fluid and electrolyte balance.
Anatomy of the Urinary Tract
The urinary tract is a pathway that carries urine out of the body. It includes:
- Kidneys: Two bean-shaped organs located on either side of the spine, below the ribs. They filter blood and produce urine.
- Ureters: Two muscular tubes that transport urine from the kidneys to the bladder.
- Urinary Bladder: A hollow, muscular organ that temporarily stores urine.
- Urethra: A tube that carries urine from the bladder to the outside of the body.
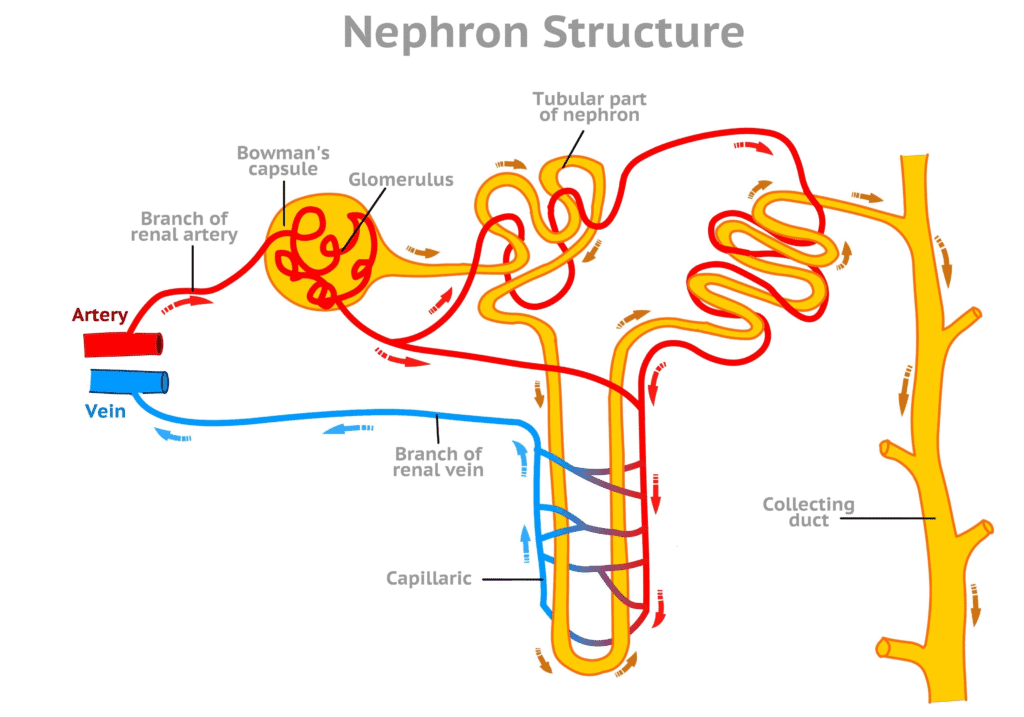
Kidney & Nephron Structure
The kidney has a complex internal structure consisting of an outer cortex and an inner medulla. The medulla contains cone-shaped structures called renal pyramids. The functional unit of the kidney is the nephron. Each kidney contains over a million nephrons, which are responsible for forming urine. A nephron has two main parts:
- Glomerulus: A network of capillaries where blood is filtered.
- Renal Tubule: A long, coiled tube that reabsorbs essential substances and secretes waste products, ultimately forming urine. The renal tubule consists of the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule.
Functions of the Kidney & Urinary Tract
The kidneys perform several vital functions:
- Excretion of Waste: They remove metabolic waste products like urea, uric acid, and creatinine from the blood.
- Fluid and Electrolyte Balance: They regulate the body’s water content and the concentration of electrolytes like sodium, potassium, and calcium.
- Acid-Base Balance: They maintain the pH of the blood by either reabsorbing bicarbonate (HCO3−) or secreting hydrogen ions (H+).
- Hormone Production: They produce hormones like erythropoietin, which stimulates red blood cell production, and renin, which helps regulate blood pressure.
Physiology of Urine Formation
Urine formation is a three-step process that occurs in the nephrons:
- Glomerular Filtration: Blood is filtered in the glomerulus. Water, ions, and small molecules are pushed out of the blood and into the renal tubule, forming a substance called filtrate.
- Tubular Reabsorption: As the filtrate moves through the renal tubule, the body reclaims essential substances. Over 99% of the water, glucose, amino acids, and some ions are reabsorbed back into the bloodstream.
- Tubular Secretion: The kidney actively secretes waste products and excess ions from the blood into the filtrate, further fine-tuning the composition of the urine.
Kidney in Acid–Base Balance
The kidneys are crucial for maintaining the blood’s pH within a narrow, healthy range of 7.35 to 7.45. They achieve this by:
- Secreting Hydrogen Ions (H+): When blood pH drops (becomes too acidic), the kidneys excrete excess H+ ions into the urine.
- Reabsorbing Bicarbonate Ions (HCO3−): Bicarbonate acts as a buffer. When blood pH is low, the kidneys reabsorb more HCO3− from the filtrate back into the blood to raise the pH.
